increases the chance of a healthy birth per embryo transfer.
Increases the chance of a healthy birth per embryo transfer
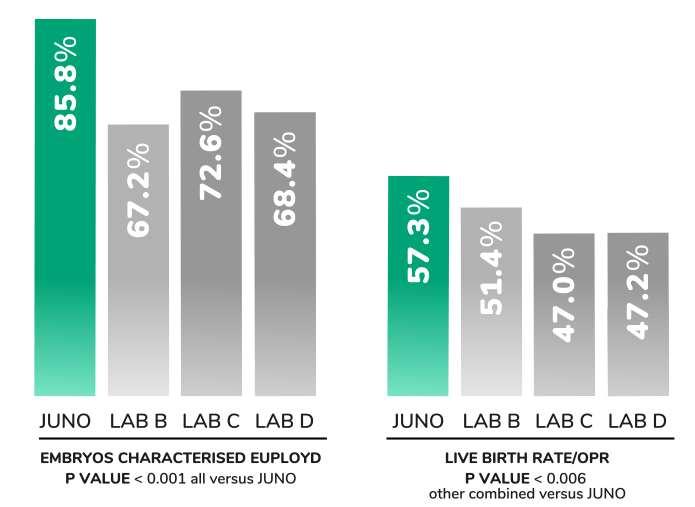
The best-in-class accuracy of PGTseq-A means an increased number of euploid embryos are correctly reported, leading to more viable embryos being transferred with higher pregnancy rates than is achieved using less accurate PGT-A methods.
More embryos are reported ‘euploid’ using PGTseq-A compared to some other PGT-A methods
Unlike most other methods, PGTseq-A combines two distinct pieces of information to provide unparalleled accuracy. The test simultaneously assesses the quantity of DNA at thousands of sites on each chromosome using an advanced next generation sequencing method. The test also evaluates numerous variations in the DNA sequence, known as single nucleotide polymorphisms (SNPs). Together, these two pieces of information provide major advantages over other PGT-A methods, including the detection of triploid embryos. The PGTseq-A technology is the most accurate test of its kind, with proven clinical validity.
– The most powerful embryo selection tool
– The most accurate and highly validated test of its kind
PGTseq-A method provides two pieces of information:
Quantity of DNA measured at thousands of individual sites
Genotypes determined for thousands of DNA polymorphisms
– Avoid unsuccessful transfer of non-viable aneuploid embryos
– Reduced miscarriage rate
– Reduced risk of aneuploid syndromes
– Faster time to pregnancy
– Permits high efficiency single embryo transfer (SET)
– Accurate detection of triploidy
– Avoids incorrect ‘mosaic’ designation
– Higher proportion of embryos classified ‘euploid’

Juno uses a unique PGTseq-A methodology, which has successfully demonstrated clinical validity in a non-selectin study
Our PGTseq-A technique employs the latest next-generation sequencing methods, increasing the quality of the data obtained and yielding results of unparalleled accuracy
Juno uses next-generation sequencing to measure the amount of DNA at thousands of sites on each chromosome. This allows the number of copies of the chromosome to be calculated with high accuracy.
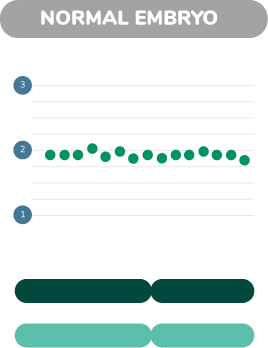
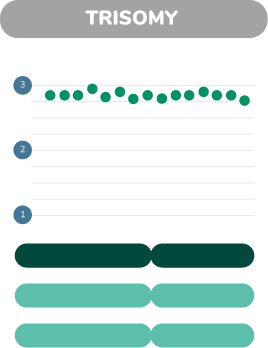
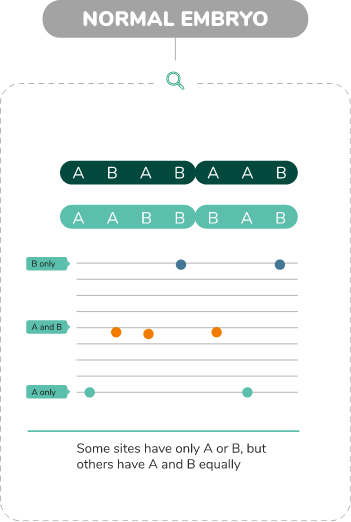
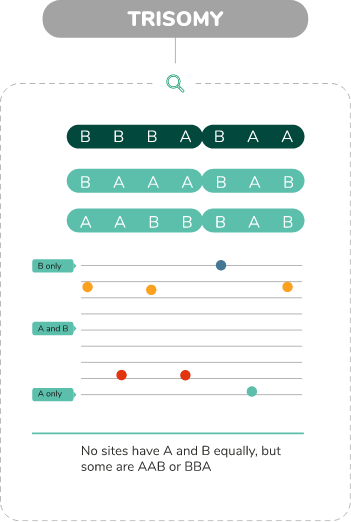
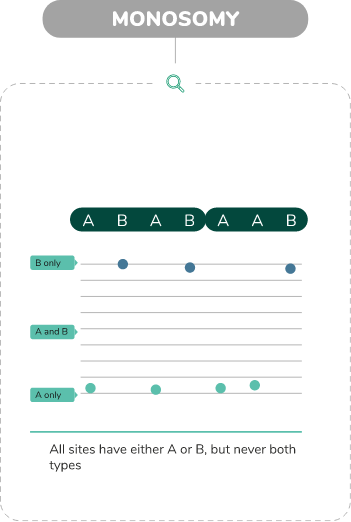
Juno looks at thousands of places where the DNA sequence can differ between individual chromosomes. Each of these sites of variation can be type ’A’ or type ‘B’. Normal, Trisomy and monosomy each have characteristic patterns of As and Bs.
Together, the measurement of the amount of DNA and the analysis of the DNA sequence greatly increases the accuracy of PGTseq-A
Juno PGT[A]Seq increases the chance of a healthy birth per embryo transfer
Biopsy and embryo vitrification
PGTseq-A
RESULTS 5-10 days
Transfer of normal frozen embryos


25,007 embryos analyzed.
%transferable per informative embryo
The enhanced accuracy of PGT[A]Seq prevents viable embryos from being incorrectly classified mosaic.


25,007 embryos analyzed.
%transferable per informative embryo
An increasing number of IVF cycles include PGT-A to assist in the selection of euploid embryos for transfer to the uterus. All modern PGT laboratories utilise next generation sequencing (NGS) to predict the copy number of each chromosome. Given this technical convergence, it has generally been supposed that the choice of PGT-A provider need only depend on factors such as the quality of the user experience, convenience and price. Here we consider whether the choice of PGT-A provider might have more profound affects, potentially impacting clinical results.
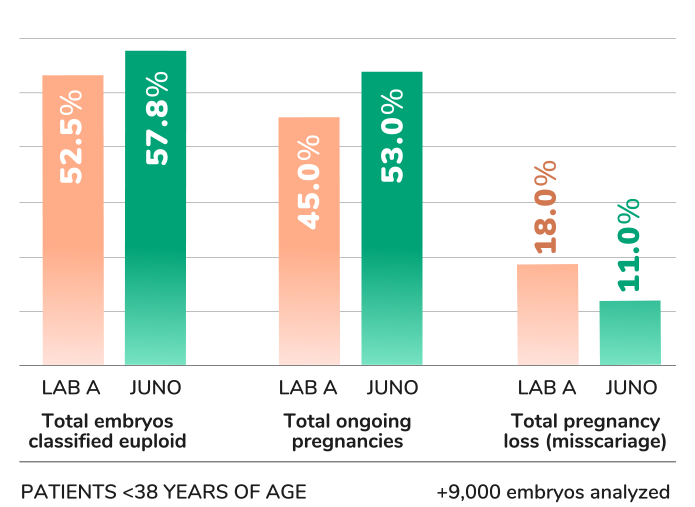
A large network of IVF clinics switched from PGT-A provider ‘A’ to provider ‘B’. The final 6 months of clinical data using A was compared to 6 months of data after the switch to B. No significant changes in any aspect of patient population, treatment or embryological practice occurred between the two time periods evaluated.
Within the two time periods considered, 9,091 embryos underwent PGT-A using A and 9,550 using B. The average female age was 39.0 and 39.3, respectively. Differences in important clinical outcomes were observed, which were particularly apparent for female patients <38 years of age. For that group, A versus B results were: 52.5% of embryos classified euploid vs. 57.8% (p<0.0001); 45% ongoing pregnancy after the first embryo transfer vs. 53% (p=0.04); 18% miscarriage rate vs. 11% (p=0.048).
PGT-A and NGS are umbrella terms encompassing different methods with widely varying levels of validation and accuracy. The results of this study suggest that the choice of PGT-A provider has implications for clinical results. One possible interpretation of the data is that higher rates of euploidy and pregnancy with B might be a consequence of embryos being wrongly classified as aneuploid by A, while incorrect labelling of abnormal embryos as euploid could explain the relative increase in miscarriage rates when using that provider.
The enhanced accuracy of PGT[A]Seq prevents viable embryos from being incorrectly classified mosaic.
All couples undergoing IVF have a high likelihood that some of their embryos will be aneuploid. Such embryos typically fail to implant, miscarry, or more rarely produce abnormal pregnancies affected by problems such as Down syndrome. Consequently, PGTseq-A is likely to have value for all couples. However, testing chromosomes in embryos becomes progressively more important as women age. By the age of 35 it is typical for more than one-third of embryos to be aneuploid, and by the time a woman is over 40, more than three-quarters of embryos are chromosomally abnormal.
Chromosome abnormalities are invisible without using specially designed tests. PGTseq-A is the most accurate method for distinguishing embryos that have the potential to form a healthy pregnancy from embryos that are not viable due to aneuploidy. Identifying the embryos that are most likely to produce a pregnancy, and ensuring they are prioritized for transfer to the uterus, helps maintain the highest possible pregnancy rates when using single embryo transfer (SET) strategies to reduce the incidence of multiple gestations.